People often refer to the U.S. healthcare system as an 800-lb gorilla. Although this reference might be born out of healthcare’s size and the clout of its players, its sheer unwieldiness actually reminds us more of a wild hippo. Healthcare is big and overweight with its appetite for spending reaching new heights every year, and it’s also resistant to change.
According to Medicare, U.S. healthcare expenditures grew 3.7% per year between 2008 and 2013, but accelerated to 5.3% in 2014. Unfortunately, the government estimates an average of 5.8% annual growth for the next ten years. It seems that the hippo will soon be even more difficult to get under control.
The press has been quick to lay the blame on the Affordable Care Act (ACA) and rising drug prices, but spending data suggests that the problem is elsewhere. Although the ACA and the new Hepatitis C drug (Sovaldi) could be easy answers in explaining the jump in expenditures in 2014—when both were introduced to the system—they cannot explain the long-term growth. In fact, Medicare forecasts that the share of prescription drugs in total healthcare expenditures is estimated to remain around 10% per year until 2024, implying that prescription drugs will not be the main drivers of growth. Additionally, given that the ACA is designed to deliver long-term cost savings rather than short-term, it is too early to label the ACA a failure.
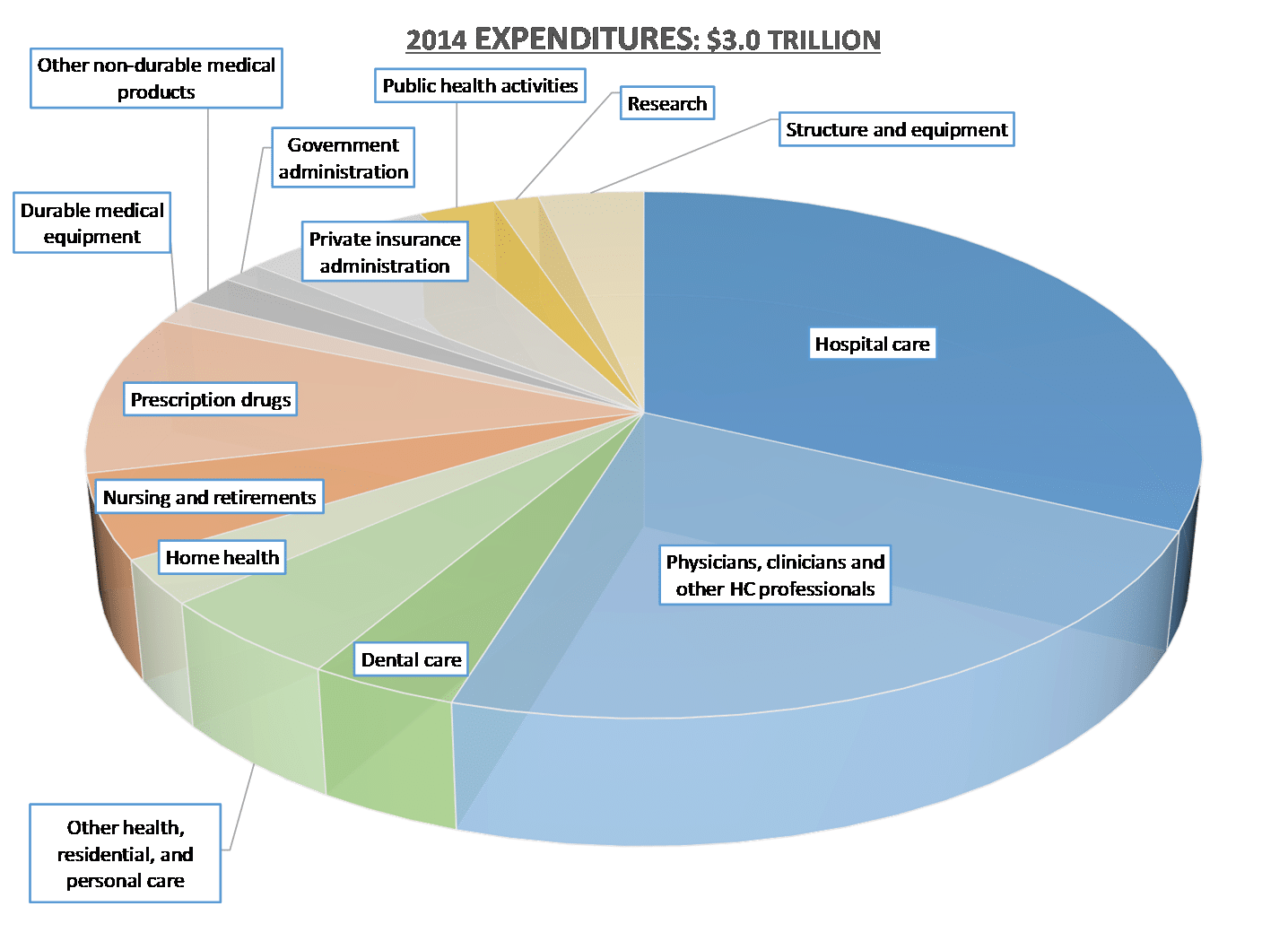
When we look at how the U.S. national health expenses are categorized (Figure 1), we see that 55% of annual costs are tied to two main categories: paying for hospital care (32%) and paying for clinical professionals (23%), both of which are expected to maintain their respective shares over the next decade. It makes sense that these two categories are responsible for the majority of spending—after all, hospitals and clinicians are the core of healthcare. But, the inconvenient truth is that if we are going to bring healthcare costs under control, spending on both will need to be meaningfully reduced.
Figure 1: 2014 U.S. Health Expenditures by Spending Categories
Source: The Center for Medicare and Medicaid Services
The theory of disruptive innovation provides a unique perspective as to why we keep spending more for hospital care and clinical professionals. Over the years our hospital systems have developed into world-class health systems, and they have done this primarily through sustaining innovations, which are based on incremental improvements of existing technologies. Hospitals today can treat many more diseases using a variety of novel technologies and methods. Imaging technology is better, surgeries are now done by robotic instruments, minimally invasive methods are used, and fully-implantable mechanical devices extend lives. Unfortunately, with each additional step of sustaining improvement in care modalities, the cost of care has also risen. Just as better products often cost more, so does better care. This is a major downside of sustaining innovations. A similar trend can also be observed among clinical professionals. As physicians specialize by gaining additional training and expertise, their services in turn become more expensive.
At the same time, since most health systems rely on third-party insurance to pay on behalf of patients, costs continue to rise. Individual hospitals (and the clinicians who work there) dictate prices, and patients consent to them. Because their insurance will oftentimes pick up the majority of their bill, and their co-pay will remain the same regardless of the overall cost, patients don’t care how much it costs. They’re essentially going “shopping with other people’s money,” as insurance companies respond by raising their premium on their members to cover the rising cost of care. Insurance companies have little incentive to push back, thus perpetuating a system that is proving to be less and less sustainable.
Given the current outlook on cost trends and cost structure of our healthcare system, the only way to shed the increasing weight is by bringing more disruptive innovations to providers and clinical professionals. Unlike sustaining innovations, disruptive innovations not only make products and services simpler and more accessible, but also less expensive. These solutions will be effective at bringing down the system cost with as little friction as possible, because disruption initially does not compete against the establishment.
So, what will disruption in healthcare look like?
Disruptive innovations will put less of an emphasis on hospital-based care and introduce new low-cost care models that focus on disease prevention and behavioral changes.
First, disruptive innovations will reduce the need for patients to access the traditional hospital system by introducing alternative clinical models. These models will be able to handle many routine healthcare services for minor illnesses such as the flu or acute cases such as broken bones. Over time, they will become better at addressing the same health problems that hospitals used to handle exclusively, but at much lower costs. Patients will no longer find the established hospital model to be the best option to deal with the majority of their health problems. Payers will be supportive of these new models, as they can curb rising premiums tied to high cost care models. They will always pay for effective care services that reduce financial burden on their members without undermining their margin.
Second, disruptive innovations will focus on curing diseases rather than treating their symptoms. Unfortunately, the established drug and device industries are more interested in extending solutions they already have in the market, even if those solutions only address the symptoms of diseases, but not their root causes. Innovators must find ways around this entrenched fad of just treating the symptoms by investing more in diagnostics that can precisely determine the causes of diseases. When diseases can be more precisely diagnosed, finding the most effective treatments becomes easier, and the total cost of care can be reduced.
Finally, we need an insurance model that will provide affordable and effective care to its members by developing a whole new reimbursement system. This will be possible only if the existing third-party insurance model is replaced with either a direct-pay or integrated provider model. A direct-pay model can bring discipline to spending by putting more responsibility on consumers and employers to decide what services to choose. Because the consumers of care are also the ones paying for it, they are more likely to make financially responsible choices. On the other hand, an integrated provider like Kaiser Permanente can control how care services are provided in the most cost-effective way, because care services are also providing insurance coverage to its patients, making them more financially responsible. Only when the third-party payer model is replaced with models that make one of the interacting parties pay, will we see a meaningful impact on the cost of care.
When we review the data, we see that the $3 trillion hippo we call healthcare is currently a very inefficient and wasteful system that is too narrowly focused on sustaining innovations. While sustaining innovations are vital for dealing with complex problems and diseases, they can be poisonous to systems with cost problems since they make costs go up. To reduce the cost of burden we must focus on developing disruptive innovations that target hospital care and physician services.