COVID-19’s toll on the US has grown more and more evident in the past several months. Lockdowns and mask mandates continue, travel across some state lines is all but banned, and experts debate whether sending kids back to school is safe. From the looks of it, things will not be returning to normal any time soon.
In March, NY Governor Andrew Cuomo called the pandemic “the great equalizer,” since anyone can catch COVID-19 regardless of their life status. While this is undoubtedly true, it downplays the disproportionate impact the pandemic is having on different communities. Low-income communities, for instance, are particularly vulnerable. Because they already face myriad social challenges, adhering to best practices regarding social distancing isn’t necessarily a top priority—not when it comes at the expense of putting food on the table. As a result, 35% of non-elderly adults with household incomes below $15,000 face a high risk of serious medical complications due to COVID-19, compared to 16% of non-elderly adults making at least $50,000 a year.
In order for healthcare providers and administrators to meet the needs of all communities, it’s essential they take social conditions under consideration as they design solutions aimed at fighting COVID-19. But to do so effectively they must first understand the circumstances and motivations that influence behavior. Enter Jobs Theory.
Jobs Theory
Jobs Theory is a framework for understanding the circumstances that drive behavior. It reveals that people rarely make decisions around what the “average” person may do in a given situation, but instead, often do things because they find themselves with a problem they would like to solve (we call this their “Job to Be Done”). Even in the same situation, two people may have different “jobs” for which they “hire” various solutions, based on their personal preferences and life circumstances.
In the context of COVID-19, Jobs Theory is a reminder that people define progress on their own terms. With this lens, a number of potential jobs that a person may have can come to light, such as, “help me feel a sense of normalcy,” “help me protect friends and family members,” and “help me keep my business up and running.”
People with these jobs may be more likely to adhere to social distancing and “hire” solutions that reduce the likelihood of contracting COVID (like working from home) since they address their Jobs to Be Done. But what about people with low incomes? Even in the face of a deadly pandemic, many may find that their jobs are still things like, “help me pay my rent” and “help me put food on the table.” To see why this is, we can look to Maslow’s Hierarchy of Needs.
Maslow’s Hierarchy of Needs and COVID-19
Abraham Maslow proposed his Hierarchy of Needs as a “Theory of Human Motivation” in 1943. His pyramid characterizes how humans tend to prioritize the progress they’re trying to make in their lives. Maslow found that people seek to satisfy needs on a higher level only when the needs on the underlying levels and foundation have been adequately fulfilled.
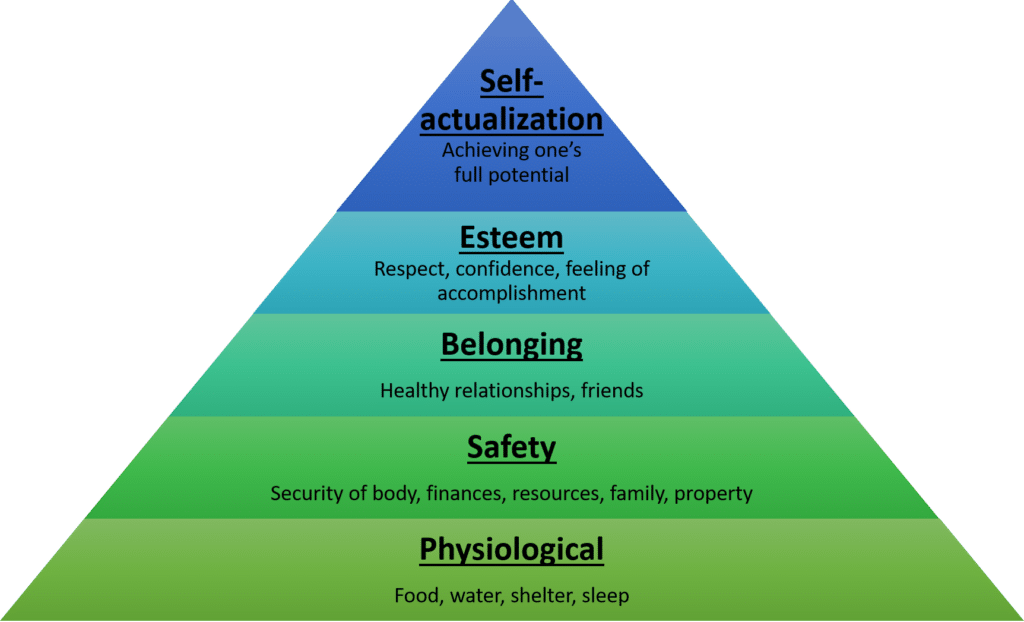
Tasks to help prevent the spread of COVID-19 fall under the “safety” section of the pyramid. These tasks may be priorities for those who already feel secure in their physiological needs, but likely not for those struggling with the basics of food and shelter. This is just one reason why communities living in poor socioeconomic conditions are sometimes forced to put themselves at greater risk. With physiological needs as a top priority, many families who lack disposable income are forced to make a variety of decisions to progress at the expense of their safety. For example, without the ability to take extended time off of work to shelter in place, many have continued to work in essential jobs. Many still rely on public transportation to get to work, and to afford housing many choose cheaper, cramped options that make social distancing impossible.
Designing solutions with patient’s jobs in mind
While COVID-19 is shedding a light on the hardships people face around housing and food security, Jobs Theory reveals that for many families, those were always top priorities in urgent need of solutions. In order to develop a society where people can focus on safety, it’s clear that people first need to have their most basic needs met. This is why US healthcare organizations interested in fighting COVID-19 must start by offering practical solutions to jobs in the lower tiers of the pyramid, and work upwards.
Some health organizations began taking steps to integrate social and community services into their practices before the onset of COVID-19. UnitedHealth provides housing to homeless patients through a new pilot program, and Oak Street Health develops processes to identify and integrate specific community needs into the care they provide, in part by hiring outreach specialists directly from the communities they serve. By addressing jobs that fulfill patients’ most basic needs, these organizations enable the people they serve to place a greater emphasis on safety measures that are critical to slowing the spread of the virus. If healthcare organizations follow their lead, under-resourced communities may become less vulnerable, ultimately benefiting everyone. Until then, only the more fortunate will be able to prioritize their safety.
For more, see:
Understanding the social determinants of health
We know we have to address the social determinants of health. Now what?



