Primary care physicians (PCPs) face tremendous pressures along the frontlines of the US health care system. Amid escalating warnings from the AMA and others about a growing primary care deficit, the need for preventative and ambulatory healthcare has never been higher. Yet while the need for more PCPs seems more critical than ever, the PCP model is under attack.
Independently practicing PCPs, in particular, are increasingly dealing with crippling overhead costs and diminishing returns. Some of these issues are rooted in new regulatory requirements involving electronic health records (EHR) and ICD-10 documentation. And inflation-adjusted reimbursement rates for Medicare, Medicaid, and private insurance are declining, so PCPs are making less money.
A New York Times article published last year paints a grim picture for the future of independent PCPs, as many feel forced to join hospital networks to relieve the financial pressures they face.
Does this mean the end of the independent physician’s practice?
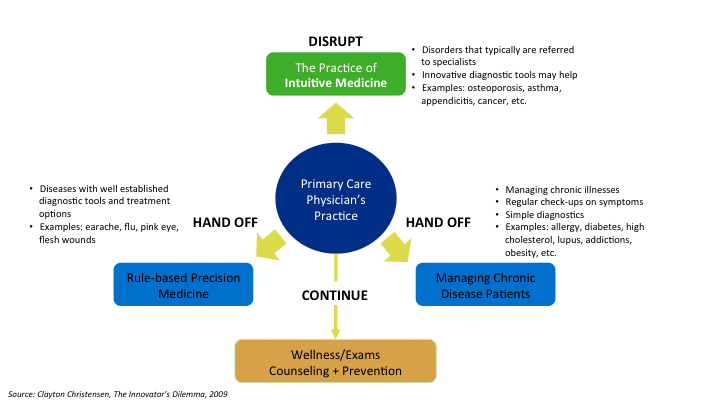
Disruptive innovation theory suggests that the future for independent PCPs is much brighter than currently advertised. For PCPs, the future lies in expanding the types of conditions they treat. Many patient examination and diagnostic functions that PCPs traditionally occupied are being taken over by RNs or commoditized on the low end with wearables or cheap, real-time diagnostics companies. Moving away from these and towards greener pastures along the fringes of specialty medicine will help preserve the PCP business model.
Patients want to consume healthcare in a number of different ways, based on the nature of the disease they experience. What a patient needs from her healthcare provider when she has the flu is very different from when she is diagnosed with early-stage Type 2 diabetes or a mental disorder. Today, advances in medical technology enable nurses to provide sufficient care for a flu patient, but patients still need the experience and training of a PCP for more serious conditions. Many of these diseases that PCPs are equipped to treat today have been the territory of the specialists in the past. But the market ecosystem for chronic disease management like diabetes received a jolt by the ACA mandated entry of nearly 40 million previously uninsured Americans. This sudden jump in patient population simply makes it impossible for specialists to handle all the care.
The key is in knowing what to hand off, what to continue treating under the roof of an independent PCP business. Herein lies the future for independent PCPs.
What to hand off. As much as 80-85% of what PCPs now do can be handled faster and more efficiently (without impacting quality) by RNs or technicians:
Rule-based Precision Medicine. Many of the categories that fall within precision medicine segment are already being handled by nurse practitioners at retail clinics or private clinics at corporations.
Chronic Disease. Chronic diseases not only require continuous monitoring but also hands-on management of patients in many cases (e.g., wound care). PCP’s time could be better spent elsewhere. However, with the rise of at-risk contracts, PCP’s will be important in managing more complex cases with multiple disease comorbidities.
What to continue. The PCP business model already aligns well with key patient needs:
General patient exams and wellness counseling. Preventative and general wellness care within the emerging ACO movement or other managed care context matches both a critical patient need with an appropriate business model.
What to disrupt. PCPs can gradually move upmarket and treat some conditions that only specialists treat now:
Intuitive Medicine. Diseases that fall within this category are often complex and require treatment by specialists. But advances in cost effective diagnostic technology and electronic decision assisting tools could allow PCPs to treat conditions that were once understood only by specialists.
In summary, PCPs do face tremendous challenges in the future – but these can also be framed as opportunities. Making smart long-term business decisions will make sense for PCPs facing increasing financial pressures. We think the best option for PCPs is to march steadily upmarket (meaning pursue both more difficult and higher margin cases) by taking on the care of patients with slightly more complex conditions along the fringes of specialty care. The increase in the number of insured will overwhelm already stretched specialists, and they will meet the PCPs with open arms. In turn, the PCPs will find a new pasture to thrive and expand their influence and reputation.