Devin Bean, a research assistant at the Clayton Christensen Institute, and I coauthored this piece.
In 2005, Rand Corporation projected widespread use of electronic health records (EHRs) could save the United States $81 billion per year in health care. Eight years later, more than 80 percent of hospitals use EHRs and have received incentive payments for their “meaningful use,” yet projected savings have still not materialized. Many blame our bloated hospitals for this disappointing shortfall.
We disagree. EHRs are not unsuccessful because of health care providers’ ineptness. Rather, they are a potentially disruptive technology that got caught in a legacy business model that can only prioritize sustaining innovations.
What makes an innovation “disruptive”?
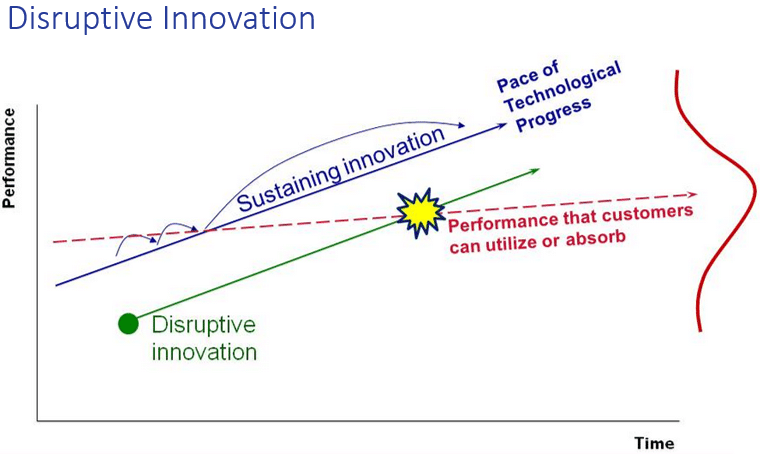
Disruption does not just mean ‘idea making waves’ or ‘breakthrough technology.’ Rather, disruptive innovation theory explains how companies with cheaper, lower performing technologies target non-consumers or low-end customer segments and grow upmarket to eventually kill larger competitors with less expensive, simpler products. The personal computer, for example, disrupted the mainframe and minicomputer industry.
In contrast, a sustaining innovation targets demanding, high-end customers with better performing, more complex products. Next year’s car model is a sustaining innovation. It’s sleek, has more horsepower than most of us could ever use, and costs more than last year’s model. Sustaining innovations result in wonderful, high performing products but not lower prices.
The reason EHRs are not “roiling the health care landscape” with disruption is not that the technology is bad—rather it’s the business model in which they are being implemented. While there is some evidence that EHRs can help increase clinical quality, the technology is by and large being crammed into sustaining business models and used as an expensive sustaining innovation to replace paper records with complex electronic systems. Implementing new technology to sustain the way you already make money almost always keeps costs high and prevents true disruption. Indeed, the history of innovation is littered with companies that had a potentially disruptive technology such as EHRs within their grasp but failed to commercialize it successfully because they did not couple it with a disruptive business model.
Business model lock-in
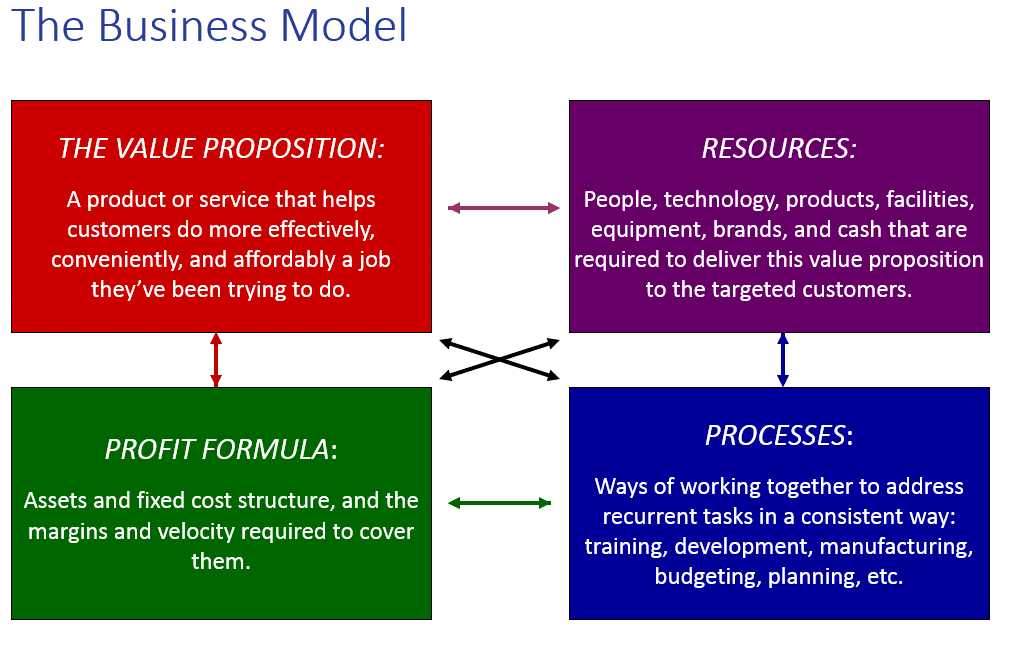
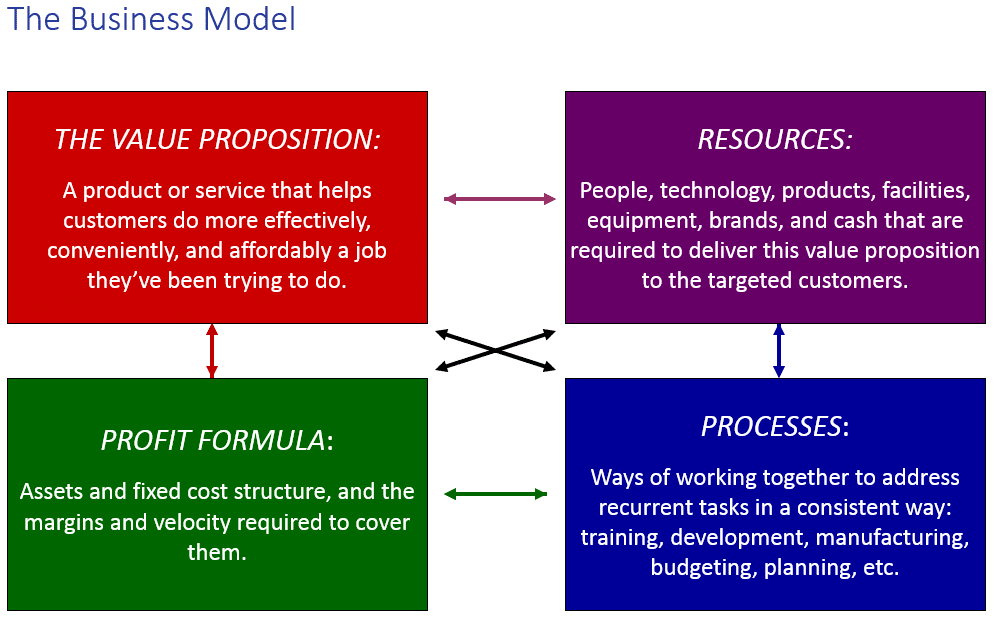
All business models begin with a value proposition, then combine resources and processes to deliver that value proposition profitably. Once profitability comes the company “locks” its business model. Business model lock-in often prevents companies from disrupting themselves because they try to use potentially disruptive technologies in sustaining ways, fitting them into their already-existing processes using their previously-arrayed resources to sustain existing profits and costs.
Nypro, a plastic molding manufacturer, saw this play out in the mid-1990s. Nypro’s value proposition centered on producing precision parts in high volumes. The CEO saw that high-volume demand was beginning to be replaced by demand for a wider variety of parts with low volume production runs. To address this emerging need, Nypro’s engineers developed a new molding machine, the Novaplast. In order to leverage existing assets, the CEO offered to lease the machine on attractive terms to his each of his plant managers.
Only nine plant managers took him up on the offer, and seven of them returned the machines after just three months.
Why did the machines fail? It wasn’t that the technology was crummy. Rather, salespeople had little reason to call on or prioritize low-volume customers when all the incentives of the sales process were aligned with turning out high-volume runs for their existing customers. Their potentially disruptive Novaplast technology got caught in a sustaining business model that was locked. Thus, the Novoplast had very little impact within the company. No one was at fault; it’s just the way that their manufacturing business model aligned.
Failure of “plug and play” EHRs
EHRs are following the same trajectory as the Novaplast machine. Health leaders see their disruptive potential. Yet most record systems are implemented as sustaining “plug and play” replacements for paper records, just as the Novaplast was implemented as a direct replacement for Nypro’s other molding machines. Clinicians using EHRs have little reason to use the new electronic system differently from the old paper system, and so EHRs often neither decrease cost nor increase quality. They’re just next year’s more expensive model of paper-based patient records.
No one is at fault; it’s just the way that the hospital business model aligns.
Recommendations
Fortunately, there are ways to avoid the trap of the sustaining business model and reap the benefits of harnessing EHRs as disruptive innovation. We offer two simple recommendations.
- EHR designers should create the systems based on the doctor’s job-to-be-done. Many EHR systems attempt to duplicate paper records, but for many doctors, paper records still cost less and are much more convenient than electronic versions. EHRs often do not conveniently provide the necessary patient information at every point in the care process. EHR designers need to think beyond fulfilling legal requirements and providing the same capabilities of a paper system to providing new and better organization, analysis, and information accessibility benefits that fit doctors’ true needs.
- EHR users must think beyond merely replacing their old record systems. By investing substantial amounts of financial and human capital in systems that do little more than replace paper records and bring in incentive money from the government, health care providers are setting themselves up for eventual failure. They will never see the promised benefits because the surrounding business model has not changed. Instead, EHR-using practices need to create teams with the authority to implement systems that use EHRs to replace not just paper-based record systems but also patient check-in, insurance processing, and all other information-limited processes. Companies such as Phreesia demonstrate how electronic records in disruptive business models could make many health care jobs simpler, lower cost, and higher quality. CVS MinuteClinic uses electronic records to not just record data, but also to guide practitioners through exams and automate peer-to-peer chart review. Facilitated networks could utilize EHRs based around patients’ needs. This type of innovation completely re-imagines the health care business model in a way that enables EHRs to keep their cost-cutting, effectiveness-increasing promises.